Control of bladder and bowel contents seems to be of a high priority to the body. The body has various mechanisms to achieve bladder control, however these don’t all have to be working optimally the whole time. It’s like having a plan A, then plan B, plan C and so on to keep you continent.
Think of it like a team that can gather around and make up for each other’s shortfalls. So if there is a continence problem, there must be several strategies that have failed for whatever reason.
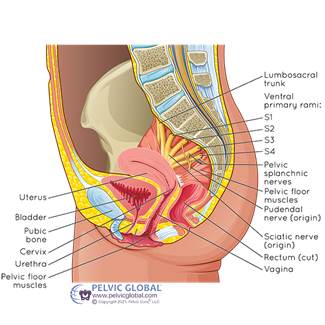
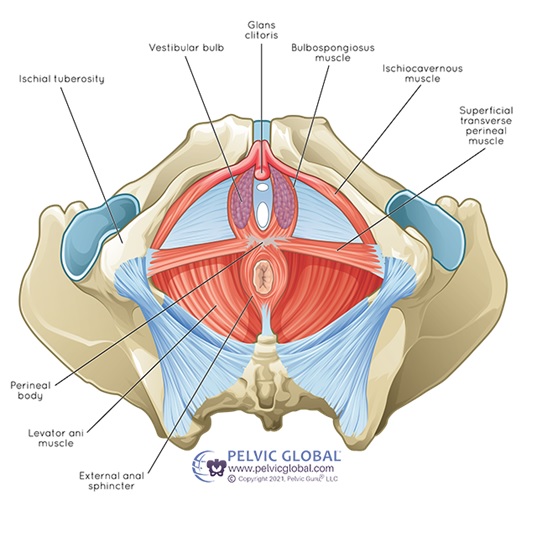
- Pelvic floor muscles. These are a sling of muscles that sit at the base of your pelvis, spanning from the pubic bone at the front to the coccyx at the back. They have several different functions to help with control of the bladder.
- The superficial layer works to squeeze closed the openings of the urethra, vagina and anus to prevent leaking of urine, faeces or wind.
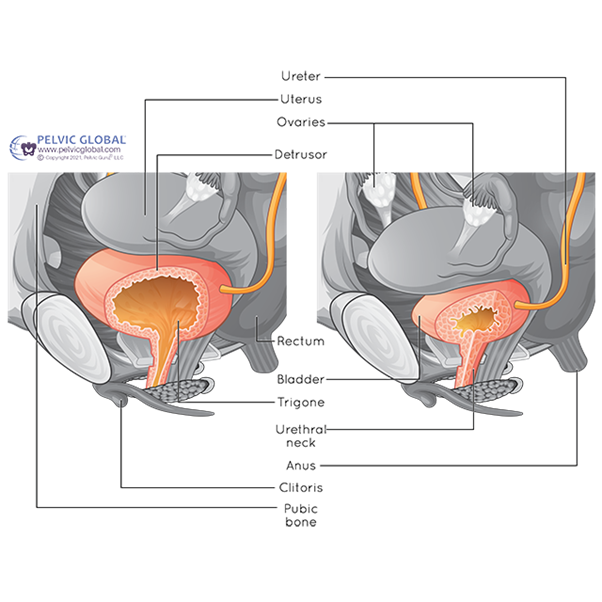
- The deep layer acts to lift the lower part of the bladder so the urethra (the tube urine passes through from bladder) doesn’t sag open at the top. Otherwise, urine would enter the top part of the urethra, stimulating the need to urinate.
- The deep layer has another function where it comes from behind to loop around the urethra, pulling it backwards and kinking it against the hard tissue adjacent. See the next section on fascia.
The pelvic floor muscles need the ability to contract with good strength, good speed, and also be able to relax and let go of the contraction at the right time.
2. Fascial support. Fascia is the spider web of tissue that surrounds everything in our body, supporting and holding it in place. Sometimes it is thin and web like. Other times it is thick and fibrous. A thick and stiff wall of fascia exists between the urethra and the vagina, called the pubocervical fascia, that has an important role in maintaining continence. As said earlier, the deeper layer of the pelvic floor pulls the urethra backward and squashes it against this pubocervical fascia. Sometimes this fascia is a bit floppy and cannot act as a hard backstop for the urethra to be pulled against. This is common in several groups:
-
- hypermobile/ very flexible people
- women who have previously difficult childbirth, perhaps causing an injury to this tissue, or even
- people who have had chronic constipation and strained to use their bowels over several years
These people can have strong pelvic floor muscles, but when the urethra is pulled backwards the urethra keeps moving too. So there is no stiff wall of fascia to kink the tube and stem the flow of urine. In these cases, it can be very helpful to have a device inserted into the vagina to provide a firm support for the urethra.
3. Mucosal lining of the urethra. The inner lining of the urethra has a sticky mucosal lining that actually sticks together and has some ability to resist unintentional urine leakage. This reduces, however, when the body produces less oestrogen such as during menopause, removal of ovaries, or during breastfeeding. In this case, the urethra can become drier on the inside, and have reduced closure pressure. This can be treated with medication if your doctor thinks it appropriate.
As I said earlier, if there is an ability to achieve continence, it probably means that there are multiple issues with the above mechanisms that have together become a problem. This means that there are multiple different treatment options to help build a bit more resilience into the system.
It is important to identify Treatment needs to be targeted towards where we can make the most impact, and sometimes we have to try addressing a range of things before
It is important to identify the main mechanisms causing stress on the system so that treatment can be targeted and effective.
Thankfully the body is remarkably resilient, and in most cases, much can be done to improve these problems.
Think of it like a team that can gather around and make up for each other’s shortfalls. Contrast this to the commonly held, but inaccurate analogy, of finding the weak or broke link in the chain.
If you have noticed changes to bladder function or pelvic floor pain, please don’t suffer in silence. Book in today to see Natasha, our Women’s Health Physiotherapist.